HPTN MODELLING CENTRE
Using state-of-the art mathematical models and data to prevent HIV
A collaborative centre that develops and uses mathematical models and cost-effectiveness analysis to support HPTN research activities and inform research directions
What we do
A 2 minute introduction to the HPTN Modelling Centre
Our preliminary results on the impact of PEPFAR cuts
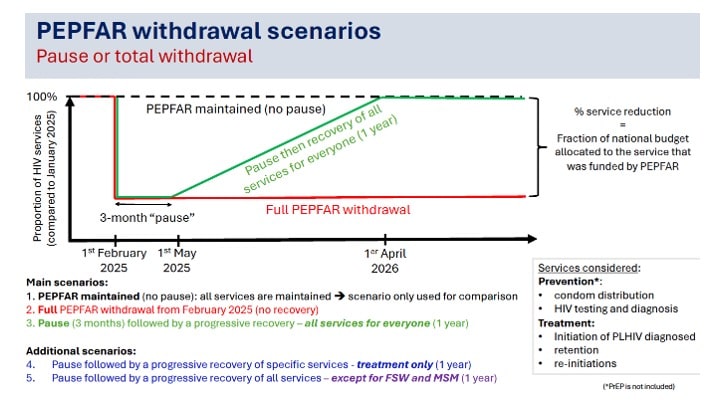
Oral presentation in Paris: Modelling the potential impact of PEPFAR withdrawal scenarios in Western Africa
Study objectives: Use a mathematical model to estimate the potential impact of different PEPFAR withdrawal scenarios in Côte d’Ivoire, Mali et Sénégal
Take-home messages
-
-
-
-
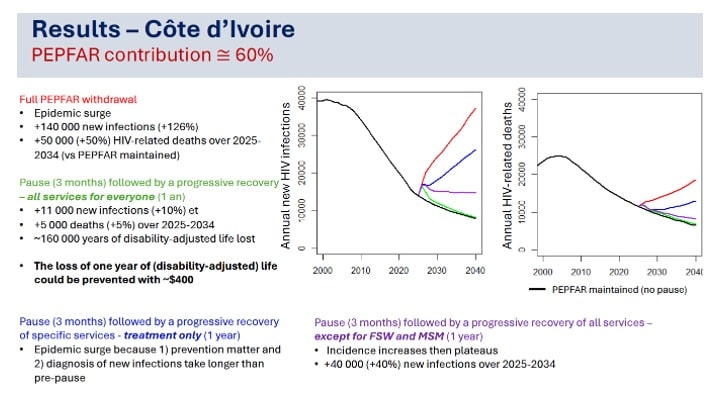
- Potentially severe impact of a PEPFAR withdrawal on HIV infections and mortality in Western Africa
- Potential increases in HIV incidence in Côte d’Ivoire and Senegal
- even if there is a recovery of HIV treatment services
- important to not overlook HIV prevention and testing
- Maintaining services towards key populations is essential
- Even a short pause could have important long-term effects on incidence
- The loss of one year of (disability-adjusted) life could be prevented with ~$500
-
-
-
Improving our understanding of the causal pathway between stigma and HIV
- Dr James Stannah poster: “Investigating longitudinal links between homophobic violence, depression, alcohol use, and HIV risk among men who have sex with men and transgender women: preliminary findings with the HPTN 075 study”

These types of analysis are important and will be used to inform mathematical models that aim to assess the population level impact of structural factors and structural enablers.
Collaboration with UNAIDS
- Our publication: Measuring HIV Acquisitions Among Partners of Key Populations: Estimates From HIV Transmission Dynamic Models
As a result of our analysis in this paper (and another collaborative study that derived estimates of fractions of new HIV infections occurring among key populations), the UNAIDS has refined their methodology underpinning their annual estimates of the fraction of HIV infections acquired by partners of key populations.
Read the full report here and watch our video on :
Our model based efficacy estimates of oral pre-exposure prophylaxis for HIV prevention in cisgender women with partial adherence
Read the details here
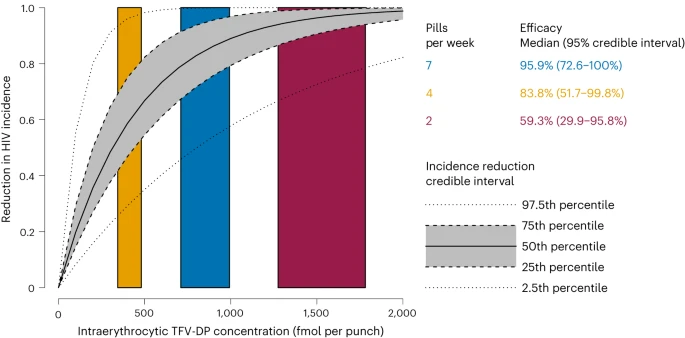
The curve suggests that high adherence confers high protection in cisgender women. However, the lower efficacy with partial adherence highlights the need for new PrEP products and interventions to increase adherence.
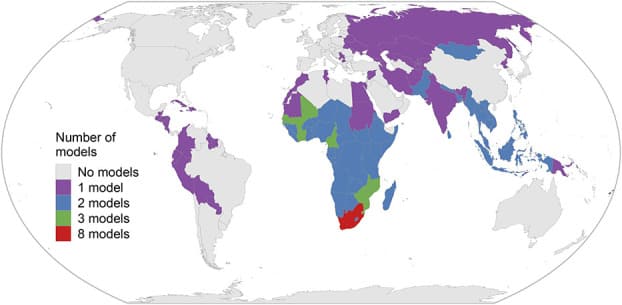
Collaborative model comparison of long acting injectable PrEP
Using models to extrapolate the results of HPTN trial (HPTN-083) into population level impact and efficiency.
You can read the full story of this analysis here
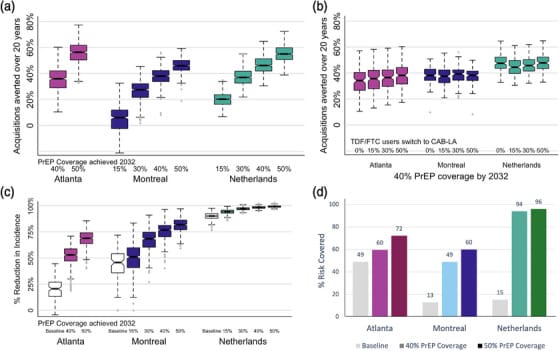
Achieving high PrEP coverage by offering CAB‐LA can impact the HIV epidemic substantially if rolled out without delays. These PrEP expansions may be efficient in settings with high HIV incidence (like Atlanta) but not in settings with low HIV incidence (like Montreal and the Netherlands).
Additional results of the Atlanta model can also be found in our Lancet Reg Health Am paper
We found that If CAB effectiveness were like HPTN 083, CAB could prevent more infections than TDF/FTC at similar usage. Increased CAB usage could contribute substantially towards reaching EHE goals, but the usage required to meet EHE goals is unrealistic.


